GMP compliance isn’t just about ticking boxes; it’s a safeguard for patient safety and product quality. One of the key elements? Identifying and managing critical findings during GMP audits—those serious red flags that indicate dangerous system failures.
This post aims to explore how organizations can effectively identify these issues during an audit, and more importantly, how they should respond when a critical finding is uncovered.
Critical findings in GMP audits
Critical findings are serious violations of GMP principles that can have a significant and immediate impact on product quality or safety, potentially compromising efficacy and endangering patients.
These issues typically indicate a lack of control, a breakdown in critical systems or processes, or weaknesses in organizational culture, and they require urgent corrective action.
Some common examples include:
- Breaches of data integrity – Falsified, deleted, or manipulated records (paper or electronic) compromise traceability and undermine confidence in product quality.
- Contamination or cross-contamination – Poor cleaning or inadequate segregation can result in unsafe mixtures of products or ingredients.
- Wrong labelling – When product content doesn't match the label, patients may receive the wrong drug or dose, with potentially harmful consequences.
- Sterility assurance failures – In aseptic environments, even minor lapses can allow microbial contamination, threatening patient safety.
- Unauthorized product release – Bypassing proper quality or regulatory checks can allow unverified products onto the market.
- Unqualified personnel performing critical tasks – Without proper training or certification, employees may unknowingly compromise production or release decisions.
Each of these findings represents a potential threat to patient safety and regulatory compliance, and each demands swift, decisive actions and proper management.
How to identify critical findings during GMP audits
Effectively spotting critical findings during a GMP audit requires a risk-based mindset, strong analytical skills, and an eye for detail. Here are four essential strategies auditors and quality teams should employ:
1. Risk assessment
Start by applying principles from ICH Q9, which focuses on Quality Risk Management. When an issue is found, ask: What is the worst-case scenario if this goes unaddressed? This helps determine the potential impact on the product and the patient, guiding prioritization.
2. Real-time operational observations
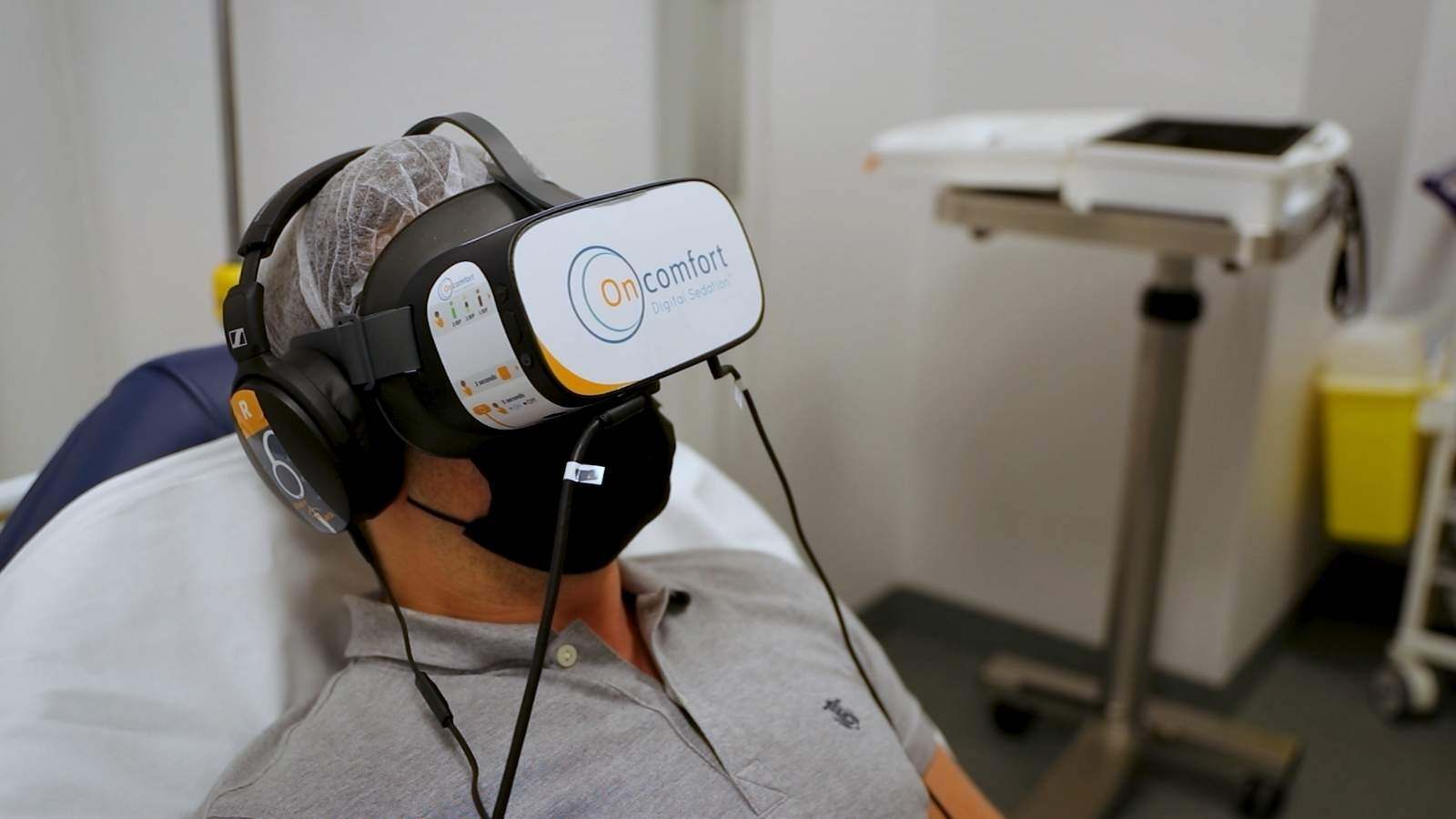
Spend time on the production floor. Are employees following standard operating procedures (SOPs)? Are aseptic techniques being applied correctly? Are labeling and packaging processes controlled? Visual observation can often reveal non-compliance that documentation may conceal.
3. Assessment of data and system integrity
Audit digital systems for access control, audit trail functionality, and data traceability. Critical questions to ask include: Who has access to modify records? Are electronic logs secure and regularly reviewed? Is the system validated?
4. Robust self-inspection program
How to Respond to Critical Findings Effectively
Once a critical finding is identified, organizations must act quickly and strategically to contain the issue and prevent recurrence.
1. Immediate containment
Stop any ongoing production related to the issue. Quarantine affected materials or products to prevent their release. Promptly inform stakeholders, including regulatory bodies if required.
2. Root cause analysis
Use structured tools such as the 5 Whys, Ishikawa (fishbone) diagrams, or Failure Mode and Effects Analysis (FMEA) to identify the underlying causes—not just the symptoms—of the problem.
3. Corrective and preventive actions (CAPA)
Develop a comprehensive CAPA plan. Corrective actions should address the immediate issue, while preventive actions should modify systems or behaviors to prevent recurrence. Assign responsibilities, set timelines, and track completion status.
4. Transparent communication
Regulators value honesty and proactive engagement. If a reportable event has occurred, disclose it promptly. Internally, keep senior leadership informed to ensure alignment and resource support.
5. Retraining and cultural reinforcement
Training is not just a checkbox—it’s a way to shift behavior and awareness. Make sure that impacted staff understand what went wrong, why it matters, and how to avoid similar issues in the future. Document all training and, where appropriate, reassess competency.
6. Follow-up verification
Conduct follow-up audits or inspections to confirm that CAPAs were fully implemented and that the issue has been resolved. This is critical to demonstrate long-term compliance and continuous improvement.
Conclusion
While no one enjoys discovering critical issues during a GMP audit, these findings can serve as powerful catalysts for improvement. When managed effectively, they lead to stronger systems, more resilient operations, and safer products. The key lies in identifying problems early, acting swiftly, and fostering a culture of accountability and quality.
Staying audit-ready isn't just a goal, it’s a mindset. By embracing transparency, risk-based thinking, and continuous improvement, companies can not only survive audits but also turn them into meaningful opportunities for growth.
Need support navigating GMP audits or addressing critical findings?
QbD Group’s experts can help you assess risk, strengthen your quality systems, and implement sustainable CAPA strategies.
Let’s work together to turn every audit into a step forward. Reach out today to take the next step toward audit readiness and quality resilience.














.png)

.jpg)