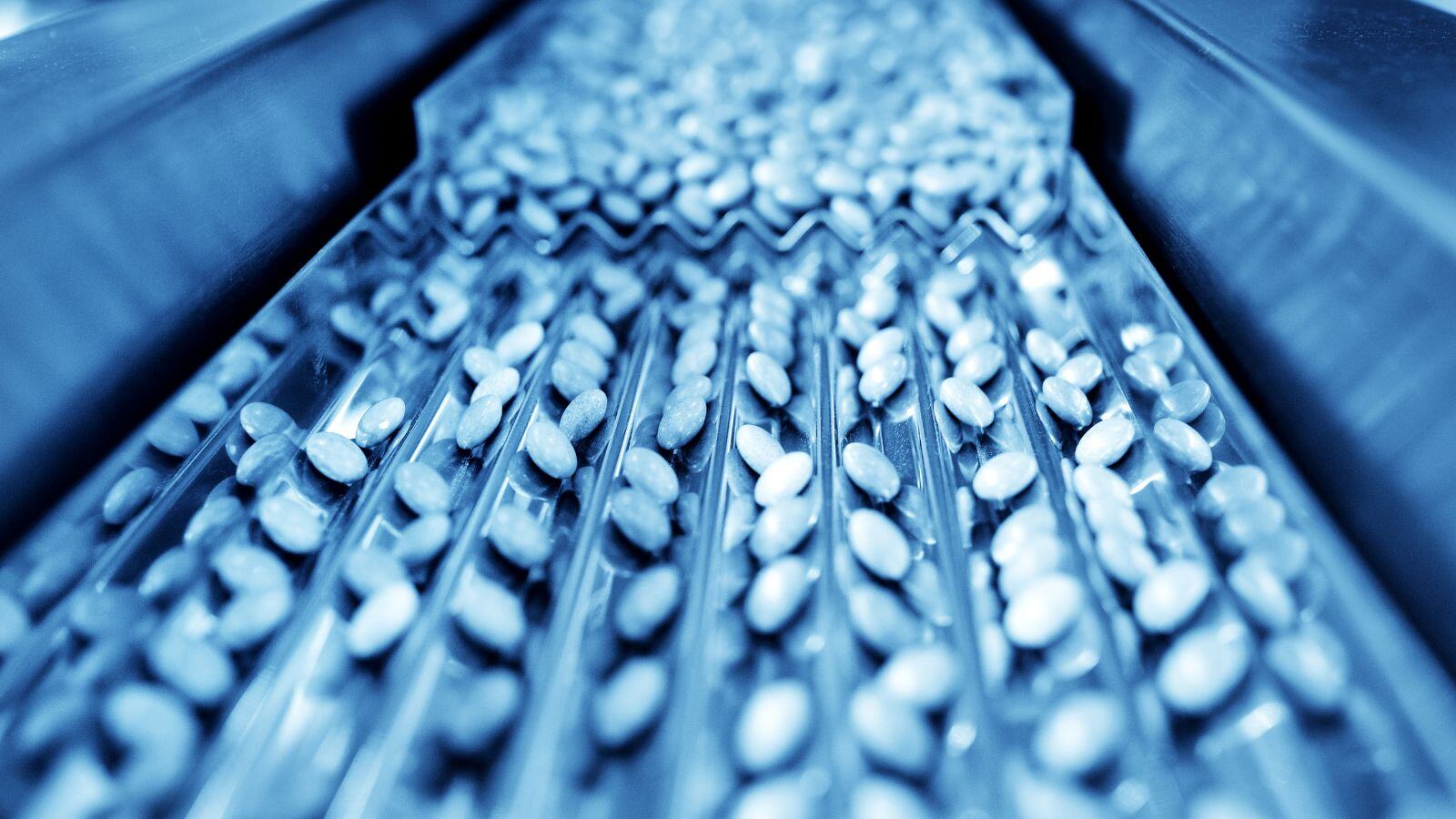
The EU GMP Annex 1 has made one message unmistakably clear: in sterile manufacturing, compliance is no longer demonstrated by isolated controls. Regulators expect manufacturers to show a joined-up system that prevents contamination, detects weaknesses early, and continuously improves.
The practical vehicle for that system is the Contamination Control Strategy (CCS), supported by an aseptic process design grounded in Quality Risk Management (QRM) and proven in routine operation.
Why does CCS play a central role in Annex 1?
Annex 1 describes the CCS as an overarching strategy that links Contamination Controls across facility design, equipment, utilities, procedures, personnel, and monitoring. CCS ensures contamination risks are managed throughout the entire lifecycle.
A CCS is not a document prepared for inspection. It is the documented explanation of how a sterile process remains in control of contaminations and how the organization demonstrates that control over time.
A strong CCS also addresses a common organizational challenge: sterility assurance responsibilities are often fragmented across QA, Engineering, Manufacturing, Validation, and Microbiology. While each function may manage its own contamination controls, no single view connects the full picture. A CCS forces that integration, making gaps visible, responsibilities clear, and remediation priorities defensible.
Aseptic process design: where strategy meets physics
The CCS is only effective if the underlying process is designed to minimize contamination risk from the outset. Annex 1, therefore, pushes manufacturers toward risk-based aseptic process design, where high-risk steps are engineered out, isolated, or robustly protected through barriers and airflow control.
In practice, this requires a clear definition of:
- Critical aseptic operations and interventions, both routine and non-routine
- The protection concept, including isolators or RABS, Grade A zoning, and transfer systems
- Contamination pathways (people, materials, equipment, air, utilities) and the controls that interrupt them
- Evidence that controls are effective in operation, not just present by design
Inspection findings frequently arise when there is a weak link between intended process design and what a site can actually demonstrate in practice.
What regulators look for and what enforcement trends reveal
Regulatory authorities demand that contamination control be both demonstrable and effective. However, enforcement trends and warning letters frequently reveal recurring failures. Common issues include weak aseptic process controls, insufficient validation of critical steps, poor oversight of interventions, and inadequate corrective actions following sterility breaches.
While challenges differ for each site, the underlying pattern is consistent: without a coherent, risk-based CCS, organizations rely on fragmented controls and reactive responses instead of proactive, risk-based prevention and continuous control.
What should a usable CCS contain?
A practical CCS enables technical leaders to answer three fundamental questions: What are our risks? What are the controls that mitigate them? How do we prove that those controls remain effective?
A concise and usable CCS typically includes:
Scope and process mapping
Give definitions of products and processes, sterile boundaries, and critical steps.
Risk assessment and rationale (QRM)
Provide clear justification for control choices, residual risks, and mitigation strategies.
Controls by contamination pathway
- Discuss facility and airflow concept, including Grade A/B strategy and pressure cascades
- Elaborate on barrier technologies, transfer systems, and intervention strategies
- Explain cleaning, disinfection, and microbial control approaches
- Unfold utilities impacting sterility assurance, such as gases and compressed air
- Clarify personnel practices covering gowning, aseptic technique, training, and qualification
Monitoring and verification
Demonstrate that environmental and microbiological monitoring provide a state of control, with governance that triggers action before failure.
Lifecycle management
Integrate the CCS with change control, deviation management, CAPA, and periodic review to keep it current as operations evolve.
Connecting CCS to Annex 1 remediation
Annex 1 describes the CCS functions as the most effective organizing framework because it naturally prioritizes effort. The different gaps identified in remediation programs will enhance your compliance level:
- Process-driven gaps point toward aseptic process design, operator qualification, and intervention control
- Facility or barrier-related gaps drive remediation in airflow protection, barrier upgrades, and smoke study evidence
- Verification weaknesses require stronger monitoring design, alert governance, trending, and investigation pathways
This is why CCS works so well as an entry point. It replaces checklist-driven remediation with a shared, risk-based structure that helps decision-makers determine what to fix first.
In summary
Annex 1 raises expectations from simply having controls to proving that controls are integrated, risk-based, and effective over time and a well-constructed CCS, anchored in robust aseptic process design, is the most practical way to meet that expectation.
It transforms regulatory requirements into an operational system that can be improved, defended, and scaled as sterile manufacturing operations evolve.
From Annex 1 requirements to practical implementation
Meeting Annex 1 expectations requires more than documentation; it requires a CCS that truly reflects how your process works in practice. QbD Group supports manufacturers in assessing, designing, and operationalizing Contamination Control Strategies that align aseptic process design, quality risk management, and regulatory expectations.
Get in touch to discuss how your CCS supports Annex 1 compliance in real life.